New Clinical Reimbursement Market Report Reveals Coordinator Strain Will Negatively Impact Reimbursement
A lot has been written about the macro trends around shifting payment models, Managed Care growth, turnover and resource strains, which continue to impact reimbursement. But not much attention has been paid to the role and function of Clinical Reimbursement. From clinical documentation to assessments to claims, clinical reimbursement ties together the elements that define financial success for a SNF.
With this point in mind, we set out to capture the key trends impacting the vital clinical reimbursement component of our business in the years ahead. The result was the inaugural Market Report: The State of SNF Clinical Reimbursement. The survey asked ~500 industry professionals to share their perspectives on top clinical reimbursement concerns, trends and strategies they plan to pursue moving forward. With the current state of the industry’s workforce crisis, it is no surprise that resource strains topped the list. However, the findings show that the staffing challenge is impacting reimbursement in a variety of ways other than just admission freezes. 90% of respondents indicated the following resource challenges will have a negative impact on their revenue potential: reimbursement staff turnover (59%), added cross-functional responsibilities such as working the floor (59%), having the time to get it right (46%) or lack of experience (42%).
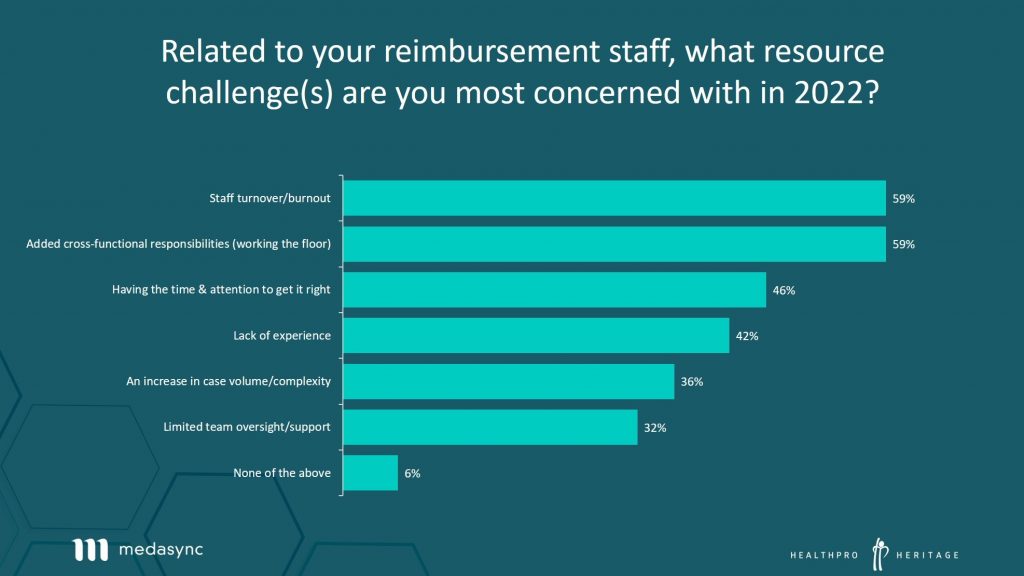
The data supports what our teams’ are hearing in the market. Resource strains have a ripple effect that impact reimbursement beyond census. Time and time again, we hear scenarios about a lack of frontline caregivers causing MDS coordinators to work the floor more and more, giving them less time and attention to perform their reimbursement responsibilities, much less get them right. The reverse is also happening, when MDS Coordinator turnover forces a Director of Nursing or a savvy nurse to pick up the slack in a role where experience, they do not have, is critical for success.
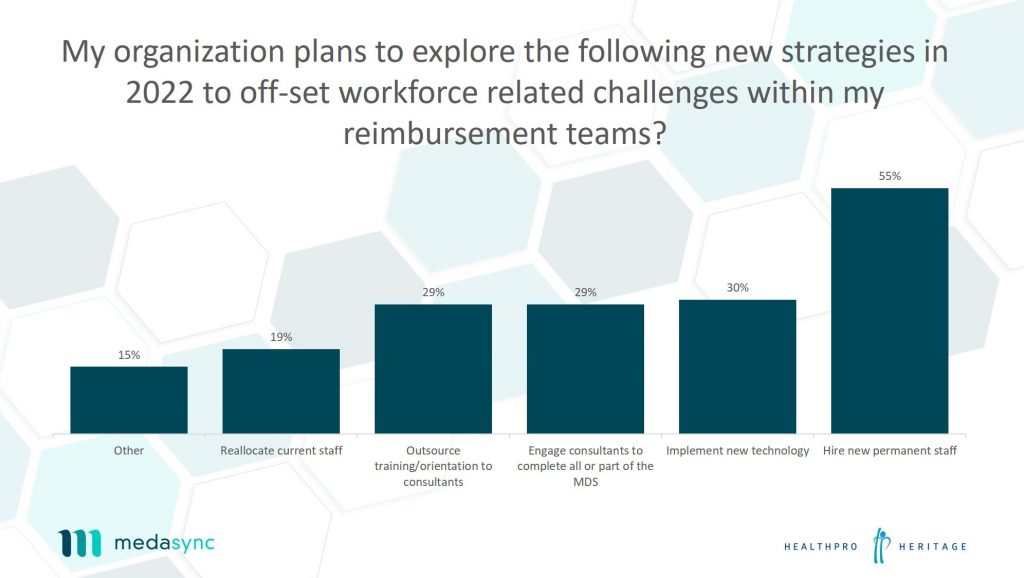
When asked about their plans to off-set these challenges, 55% indicated they planned to hire new permanent staff while 63% plan to explore help from consultants or technology to solve workforce related challenges with their reimbursement teams.
This point was further supported by a majority (65%) of respondents who expressed apprehension about their current systems and processes, while a minority (23%) expressed confidence in their current technologies. Also, when asked about having adequate resources in place to manage a multi-payer ecosystem, 75% replied that they were either moderately or very concerned.
The full survey report is available at: http://info.medasync.com/medasync-clinical-reimbursement-market-report
New Challenges Call for New Solutions.
MedaSync software and HealthPRO Heritage have partnered to drive organizational success by aligning exceptional clinical solutions with cutting edge reimbursement technology. A trusted combination to proactively ease workforce strains while impacting your reimbursement potential – helping our clients do more with less.