PDPM Medicaid Transition Playbook: 5 Best Practices for Long-Term Care Leaders
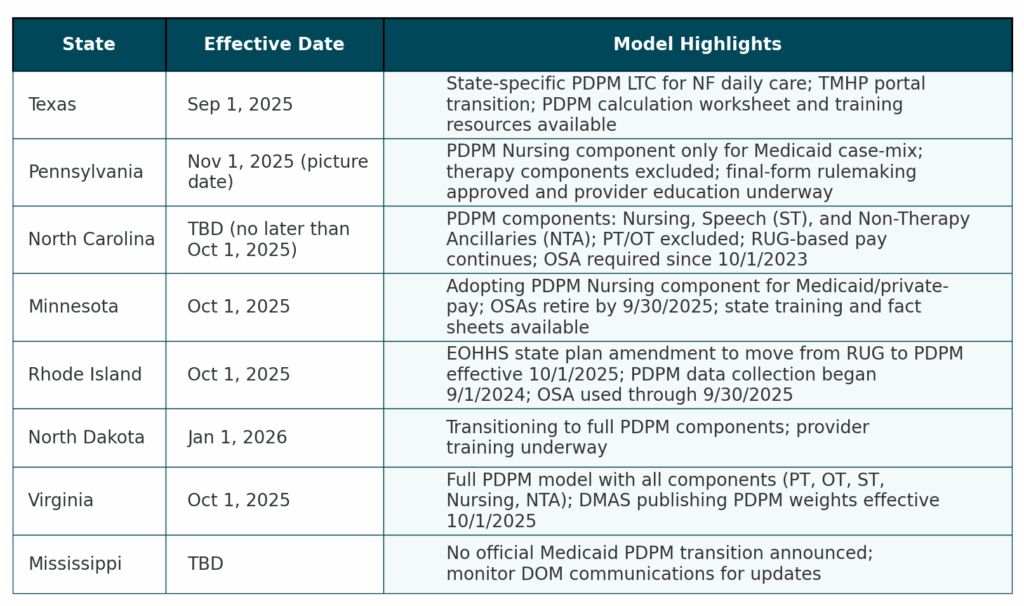
As several states prepare to transition Medicaid reimbursement toward a version of the Patient‑Driven Payment Model (PDPM), long‑term care executives must be strategic and proactive. Below, we outline the current landscape in numerous states making the switch to Medicaid PDPM, followed by five proven best practices championed by Saber Healthcare Group and Ciena Healthcare that have already navigated this transition successfully.
Five Best Practices To Prepare for Medicaid PDPM
1. Additional Training for Reimbursement & Clinical Teams
Change is a constant in the MDS world. With every change comes an opportunity to re-educate, re-train, and refocus. Invest in robust training around reimbursement drivers with a focus on the qualifiers for higher nursing components. During training you must emphasize the importance of detailed, consistent documentation especially during this transition. Saber Healthcare Group’s teams benefited from integrated sessions that included coding, clinical, and billing staff to ensure alignment on requirements and avoid missed opportunities.
Chanda Robson, VP of Reimbursement at Saber Healthcare Group, emphasized that consistent cross-training was one of the most valuable investments during their transition. “Getting everyone on the same page including key clinical, therapy, billing, and leadership stakeholders is critical,” noted Robson. “Having a software like MedaSync plays a central role in ensuring this alignment. It keeps our teams connected, proactive and helps turn our training into action.”
2. Include Medicaid Into Every Utilization Review Meeting
Medicaid residents should be a part of every utilization review meeting to catch nuances that affect reimbursement. For example, scheduling an extra OBRA assessment between quarterly MDS’s to capture a mid-period change in functional status will elevate a resident’s PDPM category significantly, translating into hundreds of dollars more per day. Technology like MedaSync’s automated chart reviews and AI-powered audits, tailored to state-specific reimbursement triggers, helps organizations streamline and scale these reviews efficiently and accurately.
Lisa Sinatra, Senior Director of Clinical Reimbursement at Ciena Healthcare, noted that, “Weaving Medicaid discussions into routine reviews shifted our culture. PDPM isn’t an isolated project, it became part of daily conversations.” Sinatra added, “MedaSync’s automation made this seamless. The system flagged opportunities we could have missed, making reviews more efficient and impactful.”
3. Renew Focus on Section GG Coding
Section GG functional coding now impacts a greater portion of the resident population under PDPM. Many organizations have adopted a multidisciplinary approach that brings together nursing, therapy, and reimbursement teams to jointly review Section GG entries and align coding with both case-mix potential and quality incentive measures.
According to Sinatra, having this collaborative approach “helps us find blind spots and ensure our coding truly reflects resident function which strengthens both reimbursement accuracy and quality outcomes.” She credited MedaSync with helping the team stay consistent, “The platform gave us guardrails, so our coding aligned with reimbursement and quality targets.”
At Saber Healthcare, the team took this even further by conducting daily Section GG charting. This proactive approach allows them to identify subtle functional changes between assessment windows that prompts timely therapy interventions and informs strategic off-cycle assessments.
4. Define an Off-Cycle Assessment Process
Not every change waits for scheduled assessments. That’s why organizations are turning to MedaSync’s intelligence and EHR-integrated alerts to determine when off-cycle assessments should be completed. These alerts surface material improvements in reimbursement without overwhelming the team with noise.
Robson explained, “The ability to identify and act on off-cycle changes is a game-changer. Without this insight, we could have left thousands of dollars on the table. The alerts made it easy to act quickly and confidently, without second-guessing.”
5. Leverage AI-Powered Technology to Guide Workflow
Hundreds of skilled nursing organizations rely on MedaSync’s AI platform, which delivers real-time, actionable alerts that are state-specific and payer-aware. These accurate alerts seamlessly integrate into the reimbursement workflow prompting timely action—ensuring every reimbursement opportunity is captured across Medicaid and all other payers.
“MedaSync took the guesswork out. It frees up our teams to focus on residents while still knowing reimbursement integrity was safeguarded,” Sinatra added. “Nothing slips through the cracks. Our workflows are stronger because of it.”
As states prepare for their PDPM Medicaid transitions, leaders can follow Saber Healthcare Group and Ciena Healthcare’s proven reimbursement strategies: team training, expanding utilization reviews, multidisciplinary GG diligence, off-cycle workflows, and smart use of AI technology. Robson and Sinatra’s experiences illustrate that success requires both process discipline and cultural alignment. Adding in a technology partner like MedaSync helps enable their teams to achieve both.
Ready to see how MedaSync can support your reimbursement team?
Contact us today to schedule a personalized MedaSync demo and ensure your organization captures every eligible dollar.