Resource Strains Threaten Reimbursement – AI Automation is a Solution
Turnover. Burnout. Staff shortages. Overtime. These are all consistent themes playing out in our nation’s nursing homes and splashed across the industry headlines each and every week. It’s not just impacting front-line staff either… Vital roles such as MDS are being pushed to the brink too. Today, if you search for MDS jobs on Indeed, you will find more than 1,700 open positions nationwide. That’s more than 1 in 10 SNFs experiencing MDS turnover.
While MDS plays a vital role in patient care and many other aspects, it’s also the backbone for our reimbursement structure. Reimbursement capture has always been a very nuanced, specialized and time-consuming job that includes daily or weekly UR meetings, tedious manual chart reviews, post-MDS audits, triple-checks, and much, much more. All of which are driven by people – staff time, diligence, and rigorous effort.
A recent survey of MDS/nurse assessment coordinators by the American Association of Post-Acute Care Nursing (AAPACN) found that more than half of respondents are overworked and 40% plan to change jobs within the next 12-months.
The risk of MDS turnover can be catastrophic for providers, with PDPM, case mix reimbursement and Quality Measures all tied to the accuracy of MDS assessments. Plus, most MDS coordinators serve managed care responsibilities too.
Growing reimbursement complexity
This strain also comes at a time when insurance complexity, across all payers, is at an all-time high. Each operator is navigating a multi-payer system unique to their region including Managed Care, traditional Medicare and Medicaid. On a county-by-county level, there are 30% more managed care plan options than there were two years ago. Traditional Medicare’s move to PDPM was a daunting task – even for the most seasoned MDS nurses and a bigger ramp-up for new ones. On top of that, state-based Medicaidprograms, whether driven by a RUGs grouper, Managed Care or some other model, aren’t the easiest systems to pick up either.
Resource Limitations + Growing Insurance Complexity = Reimbursement Risk
Given the complexity, required expertise and time-consuming nature of reimbursement, mistakes and missed opportunities were happening before our resources were strapped. Now, with our teams spread thin or lacking experience, this combination threatens to cut into our reimbursement further. Here are a few examples of the opportunity lost due to potential revenue leaks within the various payment systems:
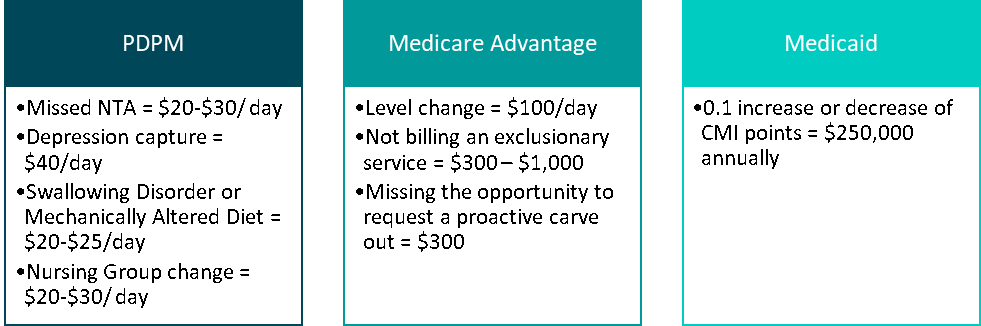
These missed opportunities may result from a myriad of things. Yes, if your team is inexperienced or new to the role, common coding mistakes will happen. However, the bigger challenge is having enough time to be proactive. With more than 68% of assessment coordinators being pulled into other responsibilities and more than half also working the floor, these resources no longer have the time to stay on top of every patient change throughout the stay. This can negatively impact timely capture, a critical reimbursement component for each payer and payment model.
Let’s consider a scenario where you have a patient condition change outside of an assessment window. Under PDPM, this will often lead to an IPA opportunity. For managed care, there may be a level increase, depending upon the plan. In certain states, this should trigger a new ARD and CMI improvement under a Medicaid RUG program. Unfortunately, none of this happens if you’re not staying on top of your case load and constantly watching for patient condition changes, which is a daunting task when your focus and attention is elsewhere. So how do you avoid the scenario of not having enough time or insight to take action?
Artificial intelligence can streamline human-tasks
Luckily, this is an ideal opportunity for artificial intelligence and new technologies like MedaSync to empower your teams. The power of AI is about freeing up people’s time to use their judgment for things computers can’t do well and employing technology to do the things that it can do better than humans. The manual task of timely capture, as illustrated above, is a good example. Here’s how cutting-edge technologies like MedaSync can efficiently stream-line this human task:
- Information gathering: Armed with advanced data mining, natural language processing and machine learning, the data side of MedaSync scans through mass amounts of patient information in the EHR, compiling utilization and patient characteristics each and every day to pinpoint condition changes or important characteristics.
- Know how: Like a human, technology can be trained to understand what’s important and what’s not. For MedaSync, this is a second layer of intelligence that processes information against a set of pre-defined payer specific rules that are uniquely important under a certain set of insurance guidelines but not all. Ie… the system is smart enough to know that an NTA doesn’t really apply in the context of a level-based Managed Care plan.
- Action: Data and information is only as good as the behavior it causes. MedaSync uses simple alert digest emails and dashboards to guide your MDS teams to focus their scarce time and attention on the right things.
In today’s environment, efficient revenue capture is more important today than ever before, especially given the immense financial pressure many SNFs are under. Without it, we can’t empower and financially support our passionate and amazing teams to keep them going and caring for the patients that need our help. Payment complexity and resource challenges will continue to intensify – and, more than ever, SNFs need the right workflows, tools, technology and support to navigate this ever-changing landscape. At MedaSync, we’re hard at work building out and refining our advanced AI solutions to supplement human expertise by automating human-tasks, supporting improvements to your workflow and revenue cycle.