Non-Therapy Ancillaries: From Complexity to Opportunity
PDPM is Here, But Are We All Aboard for the Benefit?
It’s finally January, which means most of us have survived the initial onslaught of PDPM mania. We put in the work — watched the webinars, attended the training sessions, educated our staff, changed workflows, and implemented new processes.
Preparing for the biggest overhaul in Medicare reimbursement in two decades has been stressful, and with the hard work behind us, we can walk into 2020 breathing a sigh of relief. And, many of us would be forgiven for thinking the work is over — yet it’s not. The difficult news is that many of us have only scratched the surface or tackled the basics. With the intricacies of PDPM and patient need driving revenue, coasting into the new year and not digging deeper would be a mistake.
PDPM marked a big jump in complexity. It requires staff to evaluate five times as many data points for patient condition as the old system. Mastering that complexity and tying those into revenue streams marks the next challenge. In fact, an analysis by the accounting firm Plante Moran found that an average 100-bed SNF may be leaving an extra $28 per patient day on the table — largely due to the unsuccessful capture of necessary data points. That could mean up to $122,000 per year in missed revenue for an average building.
Mastering the Complexity
While many SNFs are still navigating the change from the RUG-IV system to the new PDPM rules, others took a proactive approach. They not only began implementing processes to make their lives easier under PDPM, but they’ve also started honing in on the factors that will make them consistently successful. They’ve picked up on items such as:
- Details Matter — The proper identification of common services or conditions such as swallowing disorders, mechanically altered diets, or depression may have a $20–40 per-day impact.
- Timeliness — It’s critical to get the initial assessment right, as it will drive the reimbursement for most of your part A stays. And, considering acuity is often the highest earlier in the stay, it also may make sense to set those assessment reference dates (ARDs) sooner with heavier cases.
- Non-Therapy Ancillaries (NTAs) — There is a $24–$69 per-day difference between NTA groups. All clinical eyes must be on the patient, his or her history, medications, specialist appointments, and so on to capture the full spectrum of conditions our complex patients are presented with.
This latter item on non-therapy ancillaries is important. Depending on the patient, there is a significant revenue opportunity for your SNF that may go unnoticed. It’ll be important to pay greater attention to these factors during the admission process, leading up to the initial MDS and throughout the stay to ensure you’re not missing out.
The Non-Therapy Ancillary Opportunity
There are 50 conditions/extensive services that fall into the non-therapy ancillary category, of which 15–16 are service-driven. Each resident is categorized into one of six groupings, each with its own CMI based on:
- Bladder and Bowel (MDS section H)
- Active Clinical Conditions (MDS section I)
- Swallowing/Nutritional Status (MDS section K)
- Skin Conditions (MDS section M)
- Special Treatments, Procedures, and Programs (MDS section O)
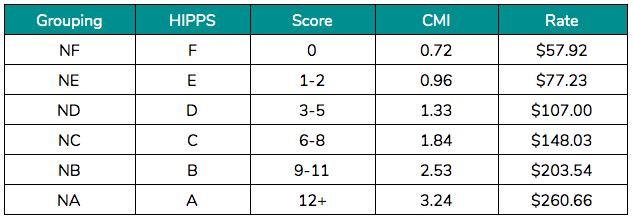
Depending on the patient and the number of conditions present, these will be summed up to produce the NTA score. Examples:
- Patient A — Active diagnosis for Diabetes that is coded in MDS item I2900 would receive an NTA score of 2 and fall into the NE grouping. Payment over an average stay of 27 days would equal $2,510.
- Patient B — Active diagnosis for Diabetes that is coded in the MDS item I2900 plus an active diagnosis for Morbid Obesity coded in MDS item I8000 would receive an NTA score of 3 and fall into the ND grouping. Payment over an average stay of 27 days would equal $3,485. The one-point difference results in an extra $975 over the stay.
Industry data suggests that 65% of historic patient stays fall into the lowest categories (NE and NF) with a score of 2 or less. Considering the industry is treating more and more acute cases, this doesn’t add up. Take a moment and look at your five-digit Health Insurance Prospective Payment System (HIPPS) codes over the last three months. If the fourth digit is all Es or Fs, you fall into that camp — and there is a good chance you’re leaving money on the table.
The Keys to Successful NTA Tracking Under PDPM
1. Diligence and Support
NTA tracking and identification is tough. It shouldn’t be, but it is. The list is long — 50 items — most of which are new. And aside from the services, many of the comorbidities need to be documented in section I8000. Unlike most of the MDS, I8000 is a blank, free-text section without the visual triggers of checkboxes that we’re used to (we know, lame excuse). But, with five times as many items to assess on the MDS, it’s easy to miss one if it’s not directly listed.
A cheat sheet listing the high impact diagnoses will be very helpful at the outset. Also, an understanding throughout the facility that change management often takes a village to support success. To that point, just about every member of your interdisciplinary team needs to understand the case management oversight required to be successful under PDPM. It will include several disciplines including admissions, clinical nursing, therapy, and physician services.
2. Workflows to Enable Proper Data Collection and Sharing
From the above, you can see the importance of aligning all teams and departments around the new PDPM rules. While they all need to understand and manage different aspects of those rules, they also need to be able to communicate and share data effectively. The coordination of the team in the first eight days of the resident’s stay will drive the reimbursement rate for most of your part A stays, unless an interim payment assessment (IPA) is completed.
Data capture and sharing should begin early in the admission process. A comprehensive analysis of hospital referral records will allow the facility to review and code the necessary characteristics. By getting the information you need from the referring hospital up front, you’ll be in a better position to start the initial assessment off on the right foot with a greater understanding of what specific non-therapy ancillaries are present. And, with this information available sooner in the process, you’ll have time to make sure ICD-10 codes have corresponding physician documentation to support that they are active.
3. Document, Document, Document
This really should go without saying, but certainly worth emphasizing. Good documentation = appropriate reimbursement. Under RUG-IV, we grew accustomed to thinking of our patients as “skilled for therapy” or “skilled for nursing.” If it was a rehab RUG, it really didn’t matter how many comorbidities each case had — the reimbursement was the same.
This disincentivized SNFs from documenting items that weren’t payment drivers, resulting in documentation that solely supported the RUG on the Medicare claim. And, this also created some bad habits that need to be broken now. Under PDPM, the days of not documenting common comorbidities — such as cardiac dysfunction, pulmonary issues, diabetes, stroke, and cognitive and behavioral changes — are long gone.
4. Timeliness
It’s critical to get the initial assessment right, as it will drive the reimbursement for most of your part A stays. And, considering patients are often at their sickest upon discharge from the hospital, the assessment may also need to be completed as early as possible within the eight-day window. This will ensure the capture of the increased acuity and higher utilization of resources upon admission.
An initial MDS assessment completed later in the window may not capture the higher NTA CMI that is usually afforded to IV infusions, medications, supplies, and nursing care if they are discontinued by that date. The cost of a missed opportunity is especially impactful as the NTA payments for the first three days of SNF stay are multiplied by a factor of three.
Get the Right NTA Tracking Solution
As with many functions within SNFs, automation and the use of technology for support will be important and beneficial to minimize manual tasks and reduce human error. That said, you don’t need complex, large-scale solutions to be successful under PDPM. The right strategic platform with the right focuses and tools may be all you need to achieve your goals.
MedaSync is a SaaS platform built specifically to support SNFs with new PDPM rules as well as existing managed care cases. Our advanced AI solutions support improvements to your workflow and revenue cycle through automated data capture pre-admission and throughout the stay. MedaSync seamlessly and electronically analyzes referral records pre-admission to ensure timely identification of PDPM drivers. The platform also analyzes and collects clinical data daily during patient stays to capture SLP, Nursing, and NTA conditions and services before the initial MDS and throughout the stay.
The power of AI is about using technology to automate or eliminate many of the manual tasks and administrative challenges we face to allow great teams to focus on delivering high-quality care.
Set up a personalized demo today to learn how you can put MedaSync to use for your SNF.